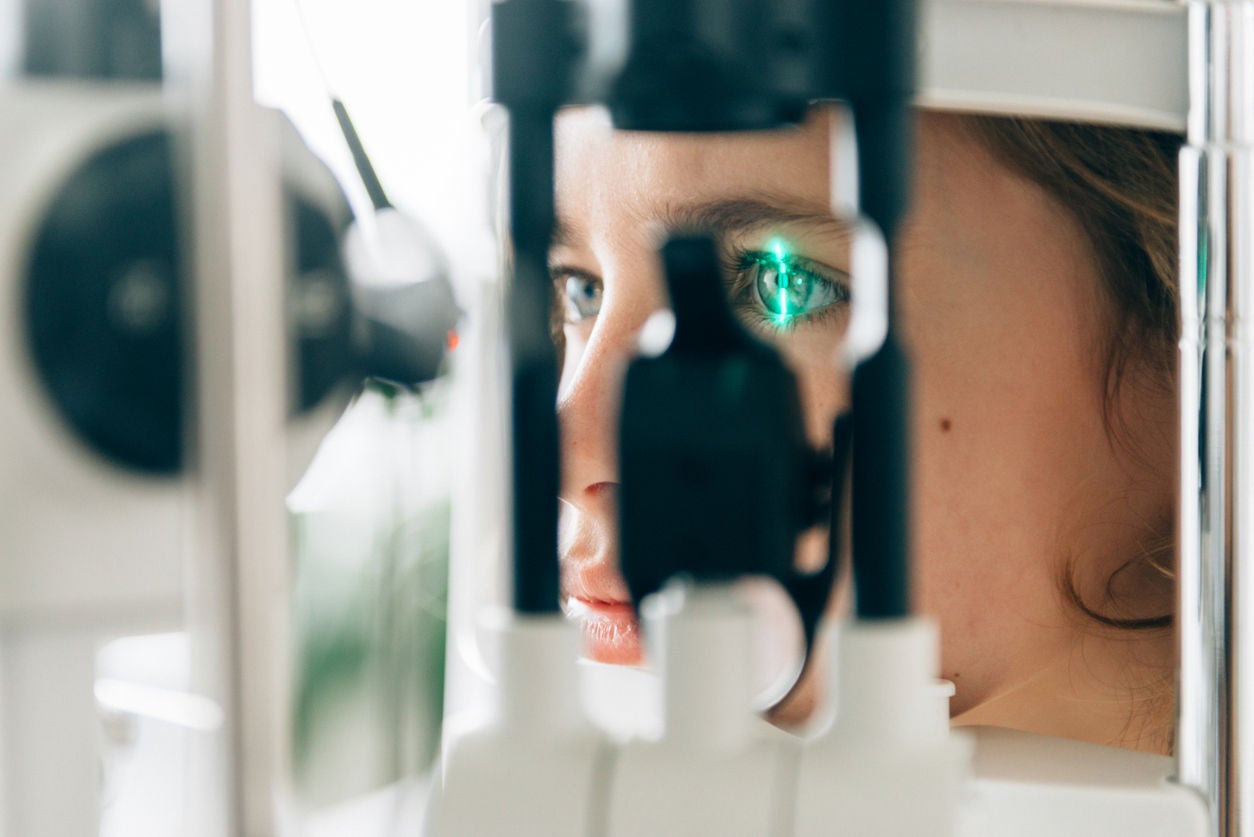
Neurotrophic keratitis (NK) is a serious eye disease that happens when nerve damage reduces feeling in the surface of the eye. Without normal sensation, the eye can’t heal properly, which can lead to injuries or ulcers that threaten vision.
NK is considered rare disease with an estimated prevalence is less than 5/10,000 individuals.